Not Just Insurance Costs, ACA Also Drove Medicare & Medicaid Costs
The short version of the Affordable Care Act (ACA), otherwise known as Obamacare, is that, while it intended to drive down health care costs by forcing more people into the risk pool and creating an online marketplace to find cheaper plans, average health insurance costs have gone through the roof.
Forcing insurance plans to cover pre-existing conditions effectively eliminated low-level catastrophic coverage plans that were significantly cheaper. Kaiser Family Foundation surveys showed average family plan costs rising by almost $10,000 since the ACA was enacted. The U.S. already had the highest health care expenditures in the world by far, and the ACA only drove them higher.
But while the rising costs of private insurance since the ACA are well established, other details of the ACA—like its restrictions on hospital payments—were supposedly keeping Medicare and Medicaid spending down.
A web page on the Centers for Medicare and Medicaid Services (CMS) site proudly claims what the ACA has done for Medicare spending by saving the agency $8 billion between 2010 and 2012 by:
…issuing new rate structures for Medicare Advantage plans, reprogramming current provider payment rates, and promulgating regulations for payment policies that will take effect for the upcoming rate year.
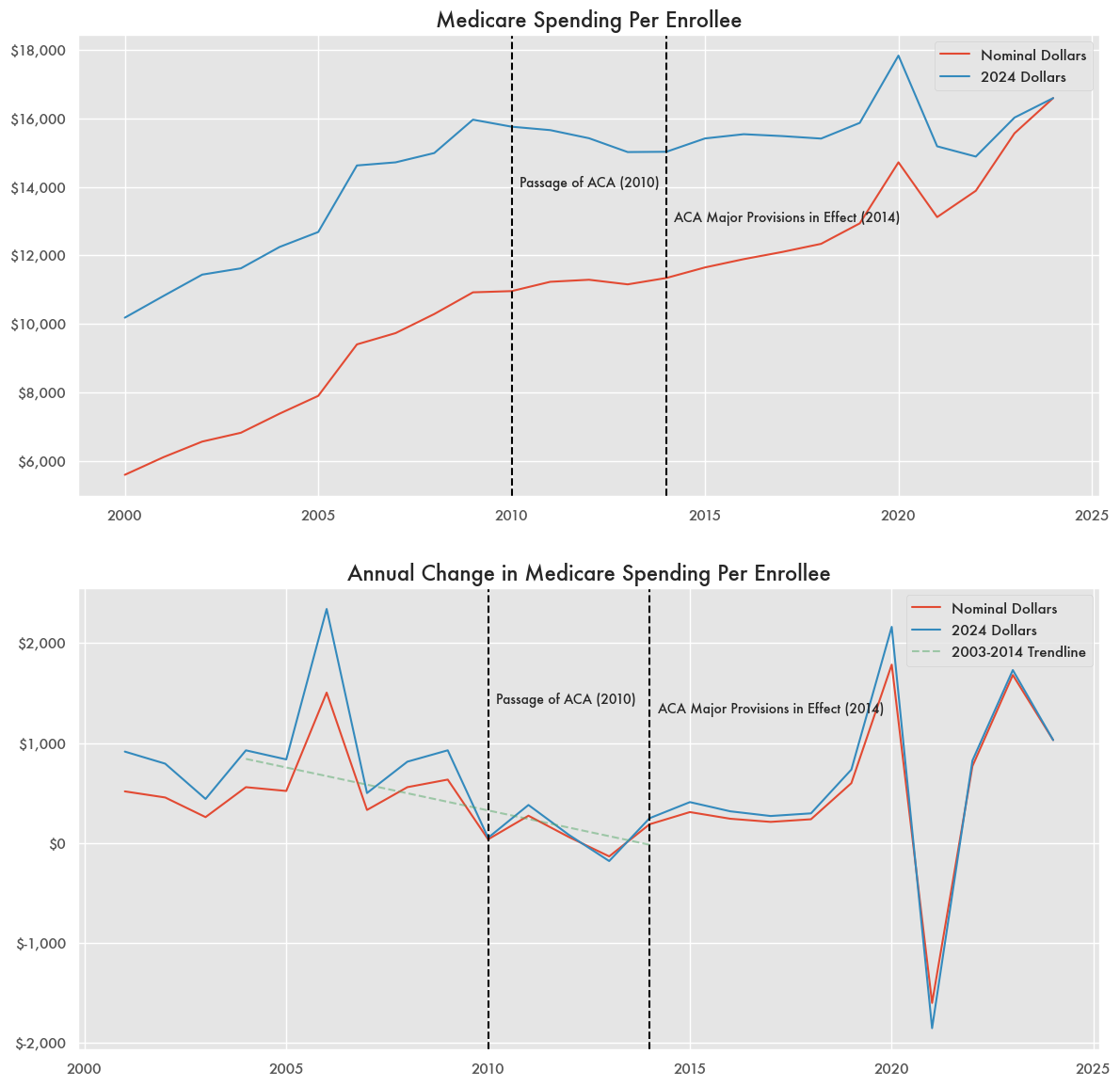
Medicare expenditures throughout the early 2000s escalated quickly as the 2003 Medicare Modernization Act (MMA) created a new prescription drug benefit option but prevented the government from negotiating most drug prices under Medicare Part D.
While the MMA drove a lot of spending, growth in Medicare expenditures per enrollee were already in decline by 2008 prior to the ACA’s passage with effectively zero growth in 2010.
The act was passed in March of 2010 and it would be highly unlikely that any of its provisions would have an immediate effect on that fiscal year’s budget, which was already half over.
Any declining growth in Medicare from the ACA’s passage in 2010 or otherwise came to a halt by 2014 when most of the other ACA provisions were in effect. Since 2014, spending increased significantly leading up to the pandemic and then again since 2023.
Medicare’s Wild Spending With Or Without ACA
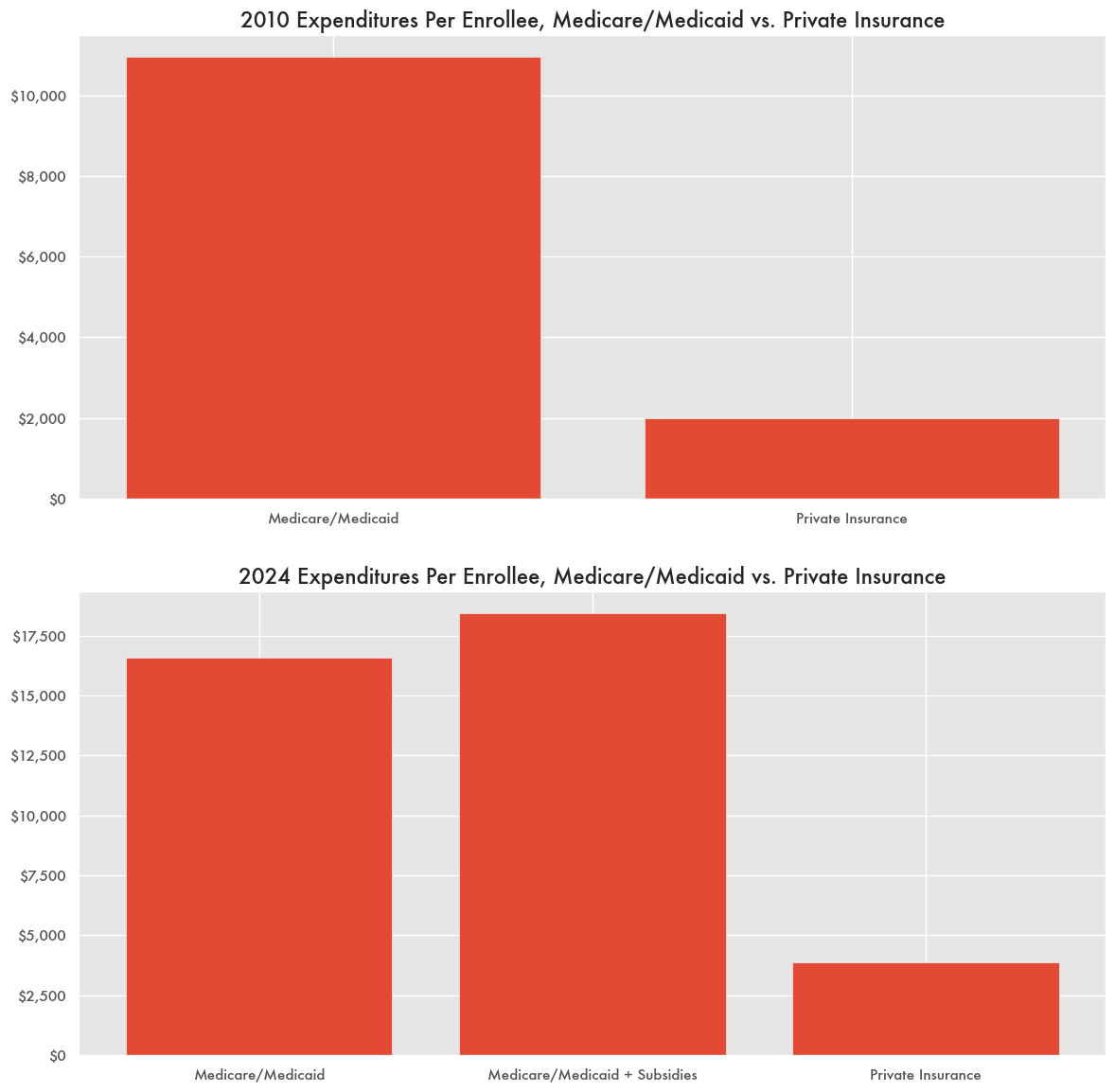
Even if Medicare’s budget had or hadn’t changed from the ACA, the program is known for being much more costly than private insurance. In 2010, expenditures per enrollee were in the realm of six times that of private insurance based on CMS and National Association of Insurance Commissioners (NAIC) report data—on the order of $11,000 versus $2,000.
With the sharp increase in private insurance costs and spending since the ACA, it’s now only about four times that of Medicare and Medicaid.
But that doesn’t include federal government spending on subsidies for private insurance like that of Medicare Advantage plans—something that came out of the ACA as well.
Those are not paid through Medicare and Medicaid, but come directly out of the Treasury’s coffers. If subsidies are included, federal government spending per enrollee is currently almost five times that of private insurance.
ACA subsidies were at the heart of the recent government budget debate that led to a temporary shutdown, and President Trump is pushing for an alternative health plan by January of 2026.

I don't mean to spam, I'm just in the rabbit hole now :)
Based on your graph (would love a link to the data to be more precise), medicare spending (in 2024 dollars) per enrollee in 2010 was about $15,800, a 55% increase over 10 years since the beginning of the graph, from about $10,200 in 2000, at a compound annual growth rate of 4.5% per year.
From 2010 to 2024, it went from ~$15,800 to ~$16,600, or only a 5% increase in 14 years, at a compounded annual growth rate of just 0.4%. If from 2010 to 2024 growth continued at the 4.5% annual CAGR from before the ACA passed, 2024 costs would be a whopping $29,300.
You are correct that Medicare enrollees are more expensive. On average, older people get sick more and need care more than younger people. Additionally, one of the key parts of the ACA was to add protections for pre-existing conditions. Previously, if you had for example breast cancer, insurers could deny you coverage. This meant that sick people were uninsured completely, through no fault of their own. Coverage for sick people is definitely higher than coverage for healthy people, but we should want all people covered. Insurance is a collective bargain - you never know when you're going to get sick.