Sudden Increase in Heart-Related Mortality Came After Prior Year Decreases
Following the sudden cardiac arrest of Lisa Marie Presley and Buffalo Bills football player Damar Hamlin, new attention is being paid to potential heart complications related to the COVID-19 vaccine and the large number of news reports of people “dying suddenly.”
While the Centers for Disease Control (CDC) recently said it would investigate safety concerns for the Pfizer-BioNTech vaccine and ischemic stroke in those 65 and older, it also said it is “very unlikely” recent concerns represent a “true clinical risk.” The CDC also stated that myocarditis—inflammation of the heart muscle that some believe is associated with the vaccine—has “rarely been reported.” Yet there are various other reports of heart ailments related to either COVID-19 or the vaccine.
But what might also be driving some speculation about heart disease and the vaccine is the sudden surge in deaths from heart disease that began in 2020.
Based on CDC data for multiple cause mortality, deaths due to heart disease in older age groups—those at least 25 and older but more prevalent in the elderly—would shoot up in 2020.
For the 75-84 age group, the number of deaths had been increasing between 7,000 to 10,000 a year from 2017 to 2019. Yet in 2020, it would increase by 54,605.
In this context, death from heart disease is defined as the following categories in the CDC’s ICD codes:
I00-I02 Acute rheumatic fever
I05-I09 (Chronic rheumatic heart diseases)
I11.0 (Hypertensive heart disease with (congestive) heart failure)
I11.9 (Hypertensive heart disease without (congestive) heart failure)
I13.0 (Hypertensive heart and renal disease with (congestive) heart failure)
I13.1 (Hypertensive heart and renal disease with renal failure)
I13.2 (Hypertensive heart and renal disease with both (congestive) heart failure and renal failure)
I13.9 (Hypertensive heart and renal disease, unspecified)
I20-I25 (Ischaemic heart diseases)
I26-I28 (Pulmonary heart disease and diseases of pulmonary circulation)
I30-I51 (Other forms of heart disease)
The sudden increase was also visible in the crude death rate—the percent of deaths per 100,000 people in that population. What was a declining or slightly increasing crude death rate in 2017-2019 (within -52.4 to 13.2 percentage point change per year) would increase by 272 percentage points.
In the U.K. a study from the nonprofit British Heart Foundation (BHF) asserted that approximately 30,000 excess heart disease deaths occurred as a result of the pandemic.
Another study in Nature pointed the blame of cardiovascular disease at climate change and rising temperatures.
A Drop in Heart-Related Deaths In Prior Years
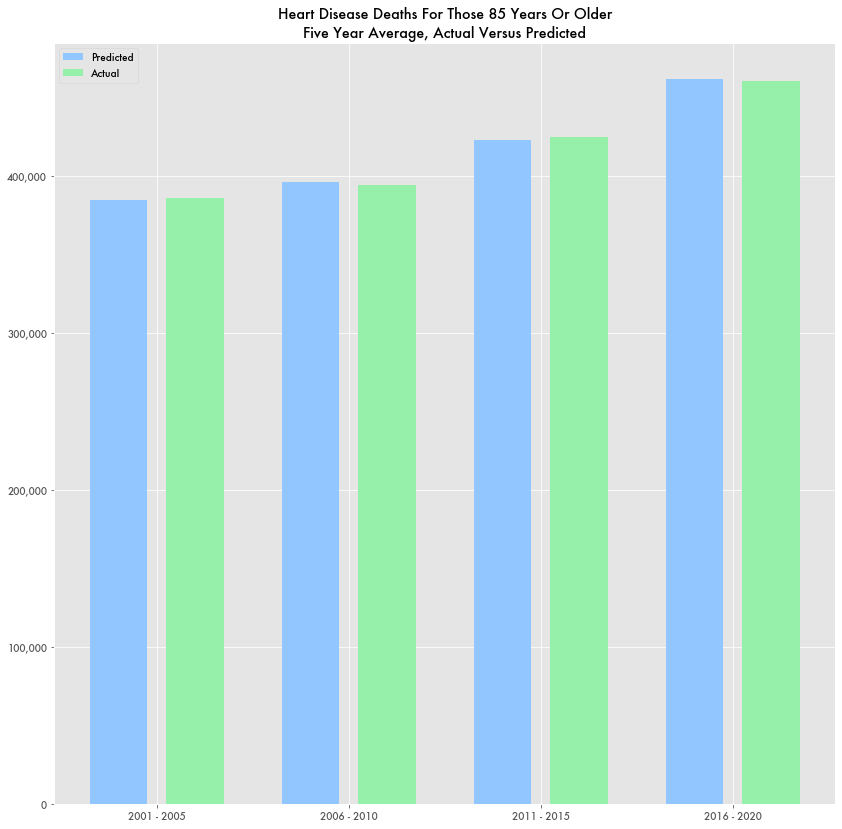
While the 2020 change in heart disease deaths is certainly anomalous, immediately prior years were anomalously low. When looking at historic data for heart disease, it’s evident that heart disease deaths hit a low point in the last decade. For the 85+ age group, it was in 2015. For the 65-74 age group it was in 2013. For 55-64, it was in 2011.
Since then it has been steadily increasing. But in 2018 and 2019, it would either stop increasing or even decrease only to sharply increase in 2020 during the pandemic.
A third-level polynomial fit of the 75-84 age group data based on data produces a good estimate through 2017—mean absolute error of 2,453 deaths, median absolute error of 1,893.
But after 2017, they diverge considerably. Average error for that age group increases 20-fold—mean absolute error of 47,296, median error of 38,560.
For some reason, deaths from cardiovascular disease would skew substantially lower
The same trend happens for the crude death rate by heart disease for age groups. It fits a third-degree polynomial through 2017 only to diverge drastically afterwards.
But in the end the total number of deaths for the last five years of data, 2015 to 2020, is almost exactly what the polynomial would predict.
That is, while the data became erratic, in the number of total deaths were in line with expectations. It’s as if the number of deaths that disappeared in 2018 and 2019 reappeared in 2020.
Similarities to Pre-Pandemic Decline in Elderly Population in Census
The decline in elderly mortality from heart disease also times with the unexpected decline in the elderly population from Census data.
A prior Investigative Economics article highlighted how the population of those over 65 began declining in 2016 after years of growth. In general, the elderly population was predicted to grow with the aging Boomer generation. The Census predicted the population to peak around 2030, not 2020.
The discrepancy between the current over-65 population and what it was expected to be based on historic trends is approximately equal to the number of over-65 deaths due to COVID-19.
Few Heart-Related Complications in VAERS Data
Health and Human Services (HHS) maintains a database, the Vaccine Adverse Event Reporting System (VAERS), that collects symptoms following vaccine administration, but there doesn’t appear to be many reports of COVID-19 vaccine-related heart complications in that data.
Certain categories could potentially be related, such as chest pain and an increased heart rate, but the most common symptoms are things like headache, fatigue, pyrexia (fever), pain, chills, nausea, pain in extremity, dizziness, and COVID-19.
COVID-19 was the second most common primary symptom. Of the 1.8 percent of COVID-19 vaccine complications that resulted in the patient dying (14,637 out of 833,463 reported events), the most common reported primary symptoms were similar: chills, headache, dizziness, fatigue, shoulder pain at injection site, and COVID-19.
In total, there are 3,393 reports of myocarditis as a symptom related to the COVID-19 vaccine. While potentially concerning, that’s not much considering that more than 256 million people have received at least one vaccine shot.
The VAERS data has a number of caveats. Anyone can submit a report, and reports are not confirmed. Symptoms are not necessarily related to the vaccine but can be conditions that existed beforehand.